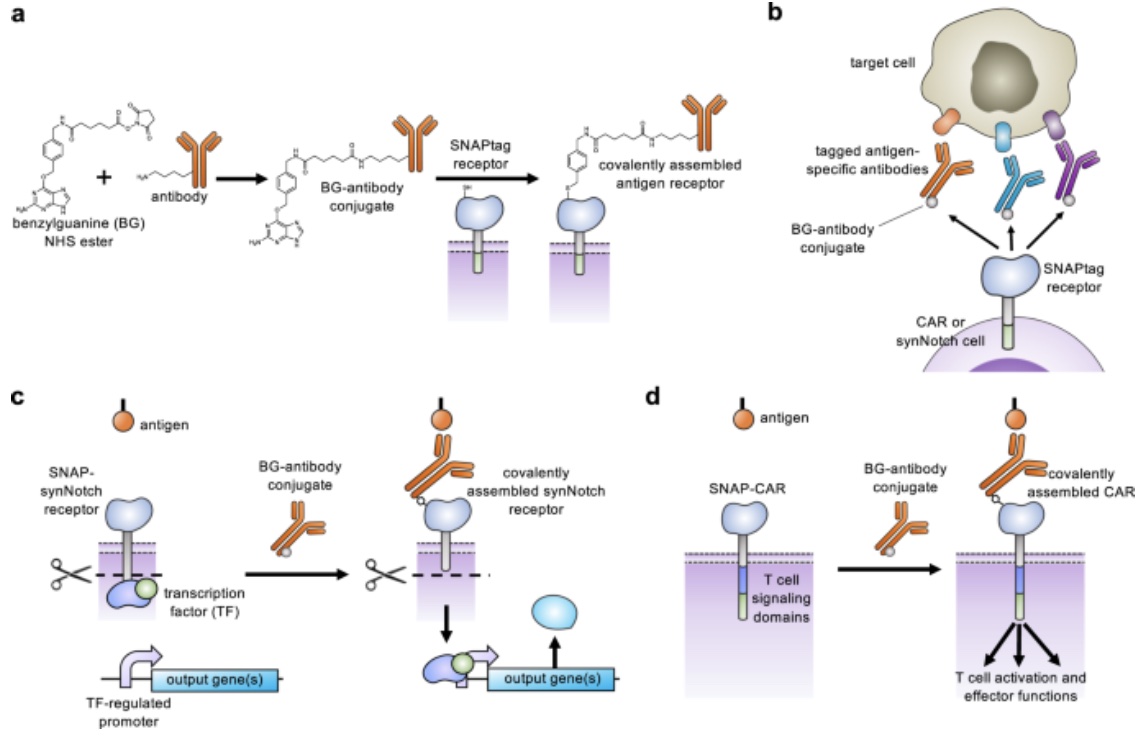
Through expanding the targeting capabilities of chimeric antigen receptors (CARs) and synthetic Notch (synNotch) receptors, University of Pittsburgh researchers have developed a “universal” receptor system that allows T cells to recognize any cell surface target. Given the potential previously seen in engineered antigen receptors, and CARs being the most clinically advanced of these technologies, the team of researchers began investigating a method to gain additional control over CAR function. By engineering T cells with receptors bearing a universal “SNAPtag”, CARs bind to the common tag molecule fused to the antigen-specific antibody, instead of directly binding antigen targets. This new approach allows for great expansion to antigen targeting and shows great promise in using CARs against additional immune-related diseases and other types of cancer.
Investigating Cancer Immunotherapy Effects on COVID-19 Outcomes
Cancer-seeking molecular delivery system could boost immunotherapy drug, research finds
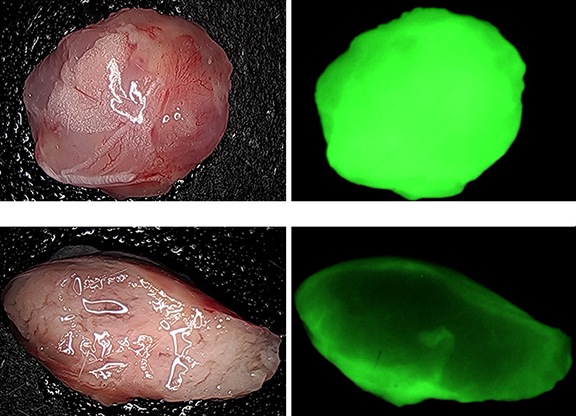
For past decades, the treatment of cancer has generally meant surgery, radiation, chemotherapy, or a combination of the above. Through recent work from a collaboration of researchers from the University of Rhode Island and Yale University comes the promising new approach of delivering immunotherapy agents, STING agonists, via a cancer-seeking molecular delivery system. The delivery relies on the acid-seeking molecule- pHLIP. These molecules deliver cargo directly to the tumor environment via targeting of the high acidity of cancerous tumors. Through this novel drug delivery technique, cancer immunotherapy may become even more effective.
Continue reading