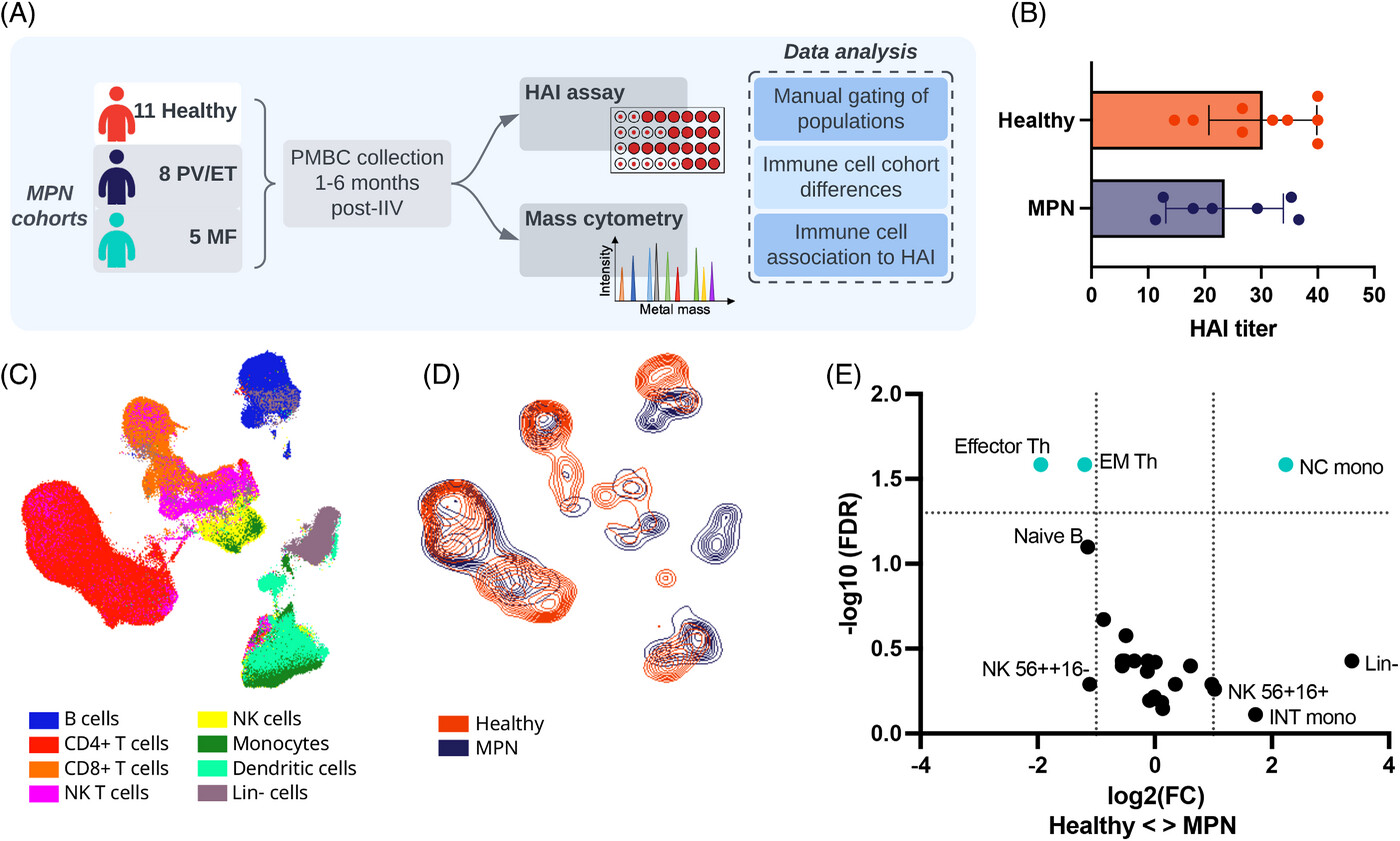
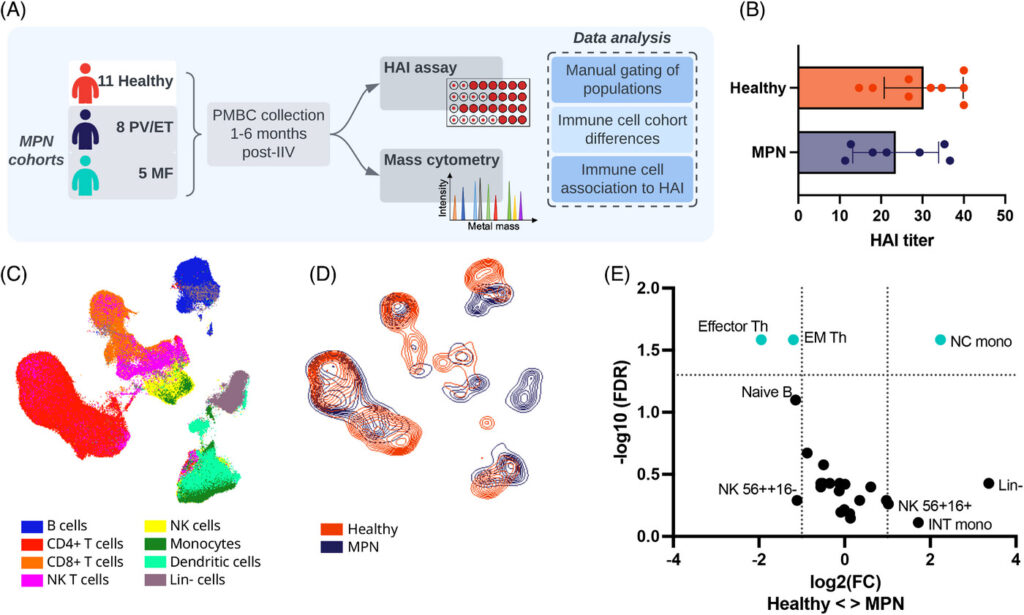
The Reeves lab recently published a study in eJHaem exploring the immune system in patients with myeloproliferative neoplasms (MPNs), a type of rare blood cancer. These patients are particularly vulnerable to infections and often require immunosuppressive drugs, highlighting the importance of effective vaccination. Our study found that MPN patients exhibit significant changes in immune cells, including decreased effector and memory T cells and reduced maturation marker expression on B cells. These changes imply that specific cells do not effectively travel to the lymph nodes for maturation, potentially leading to a compromised immune response and lower levels of protective antibodies after influenza vaccination. Our findings emphasize the need for further research into the immune dysregulation in MPNs and its impact on vaccine efficacy, aiming to improve vaccination strategies for this at-risk population.
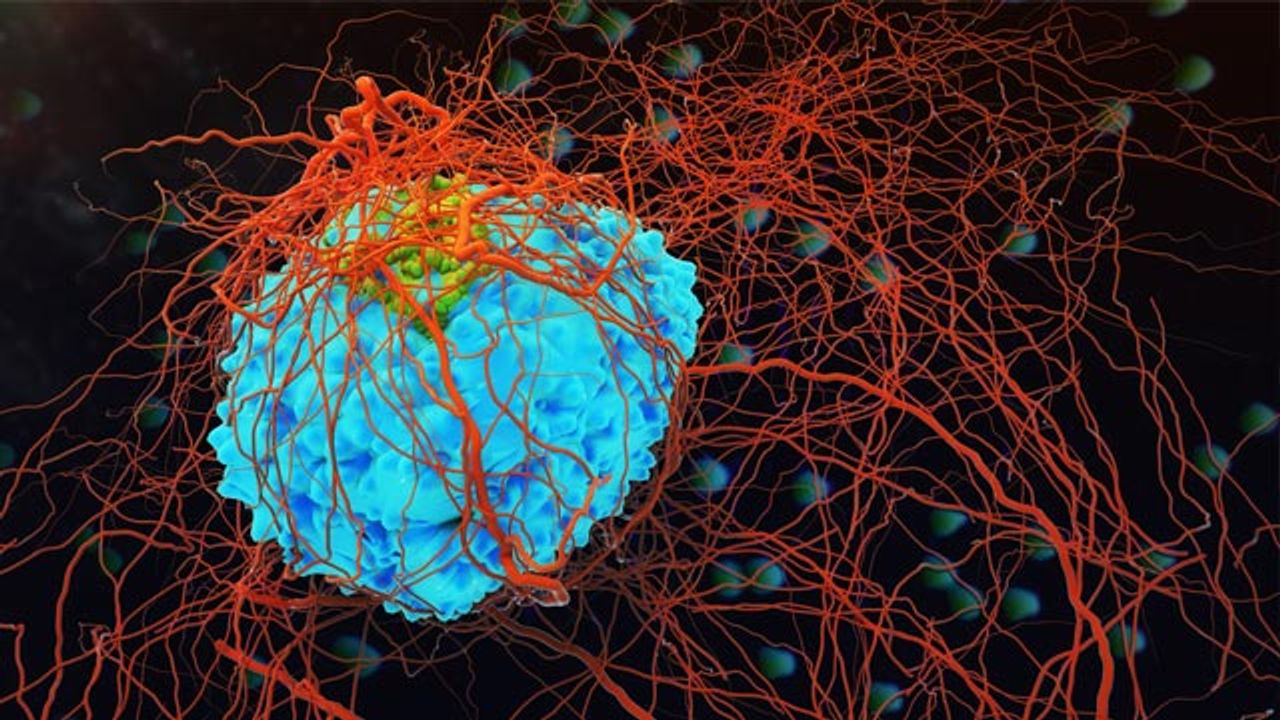
Immune cell ‘Soldier’ identified as potential target for immunotherapy
A newly discovered immune cell “soldier” may be the next target for immunotherapy. Termed killer innate-like T cells, these cells are unlike the traditional targets of immunotherapies, that is they exhaust at a slower rate and penetrate more deeply into the tissue. Killer innate-like T cells can recognize unmutated antigens and are not dependent on antigen-presenting cells. Instead the cells are constantly primed, ready to attack cancerous cells. Researchers hope these T cells, as compared to conventional T cells, may help in eliciting immune response in patients unresponsive to immunotherapy treatment.