FEBRUARY 10TH, 2023, BOSTON, MA.
HOSTED BY: THE HARVARD SAR PROGRAM, HUG, AND GMKA, IN COLLABORATION WITH HARVARD MEDICAL SCHOOL AFFILIATED PHYSICIANS AND SCIENTISTS.
Ukrainian clinicians participating in the SAR program at MGH and BWH currently, discuss their work in healthcare in Ukraine, the needs of the country’s healthcare system and ongoing challenges.
Panel of Visiting Scholars:
Sofiya Hrechukh, MD Psychiatry; Lviv; BWH
Vadym Vus, MD Family Medicine; Rivne Oblast; MGH
Ali Dzhemiliev, MD General Surgery; Crimea/Kyiv; BWH
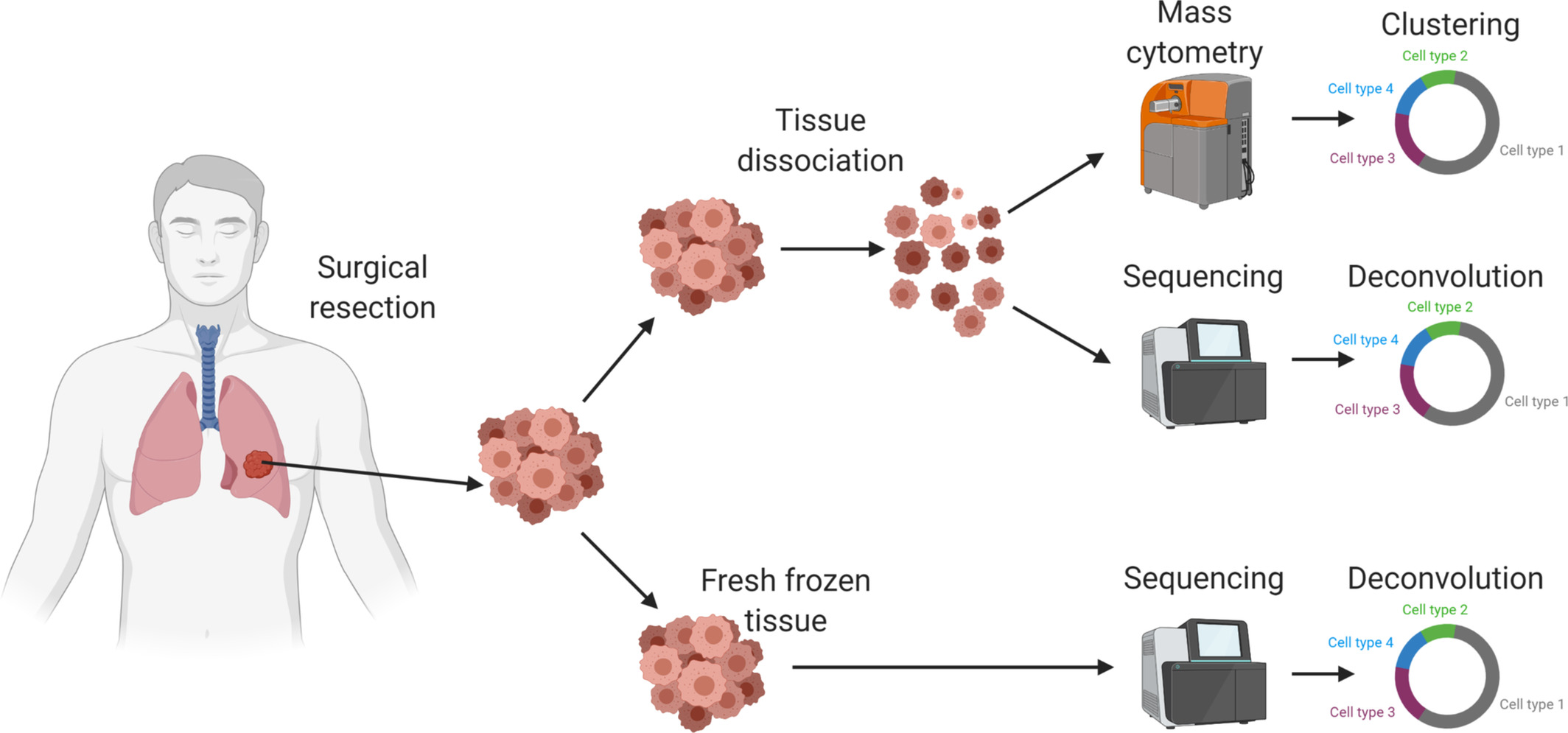
Veronika Patsko, MD Oncology; Kyiv; MGH
Moderators:
Mark C. Poznansky, MD, PhD
Director, Vaccine and Immunotherapy Center, MGH; HUG Co-Founder; Professor of Medicine, Harvard Medical School
Nelya Melnitchouk, MD, MsC
Colorectal Surgeon, BWH; Assistant Professor of Surgery, HMS;
President and Co-Founder, Global Medical Knowledge Alliance
gmka.org/
harvardscholarsatrisk.harvard.edu/
healukrainegroup.org/